Introduction
An estimated 16 million people are affected by disability due to stroke while six million deaths are recorded annually worldwide. Stroke is the second major cause of death and disability worldwide. Millions of people worldwide experience the life-altering impact of strokes, with many of them grappling with debilitating hand and arm impairments. The hand, as one of the most intricate and vital tools of human interaction, becomes a focal point of recovery.
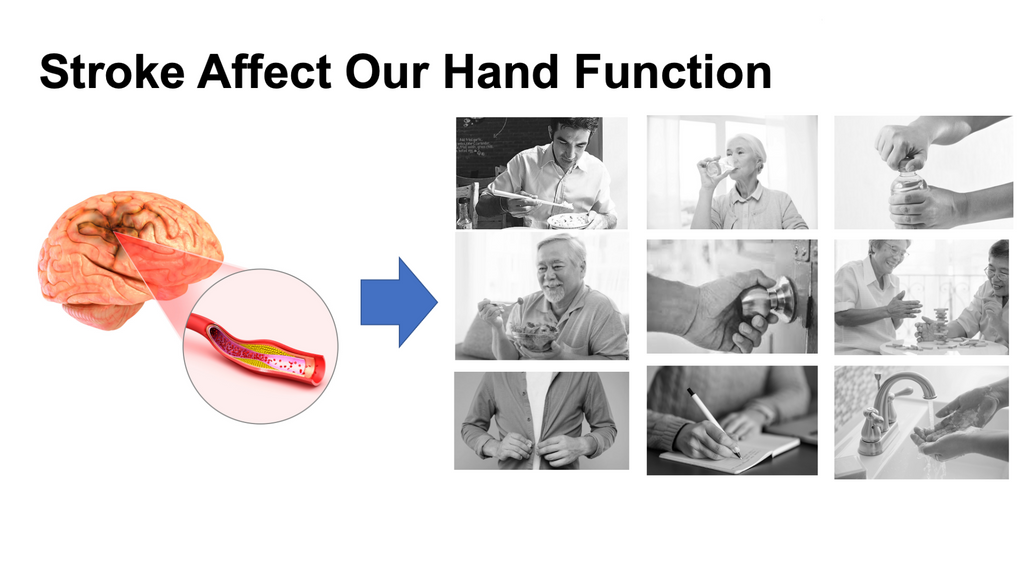
Rehabilitation of the hand is not just about regaining movement; it's about reclaiming independence, identity, and the simple joys of life - from holding a loved one's hand to performing everyday tasks with ease.
Understanding Hand Impairment After Stroke
A stroke, commonly understood as a "brain attack", occurs when blood flow to a specific part of the brain is interrupted, either due to a blocked artery (ischemic stroke) or a burst blood vessel (hemorrhagic stroke). The aftermath of a stroke largely depends on where in the brain the event occurred and the duration of the interruption. Given the intricate network of neurons and the brain's pivotal role in governing body functions, even a brief disruption can lead to lasting consequences.

The hand, with its vast web of muscles, tendons, and bones, is primarily controlled by the brain's motor cortex. Specifically, the movements and sensations of the hand are managed by a large section of the motor cortex, indicating the importance and complexity of hand functions. Post-stroke, several common impairments can affect the hand, including:
Muscle Weakness or Paralysis (Hemiparesis or Hemiplegia): Depending on the severity and location of the stroke, one side of the body might become weak or entirely paralyzed. This often manifests in the hand, making it challenging to perform basic tasks such as gripping or lifting.
Spasticity: A condition where muscles contract involuntarily, leading to stiffness and restricted movement. In the hand, this might result in a clenched fist or an inability to open the hand fully.
Sensory Deficits: Apart from motor impairments, stroke patients might also experience numbness or a reduced ability to feel temperature, pain, or touch in their hands.
Lack of Coordination (Ataxia): This involves an inability to execute precise movements, making tasks like buttoning a shirt or picking up small objects difficult.
Involuntary Movements (Dystonia or Tremors): Some stroke survivors may notice uncontrolled or abnormal movements in their hands.
Recognizing and understanding the nature and extent of hand impairment after a stroke is the first step towards effective rehabilitation. With targeted interventions and therapies, many of these challenges can be mitigated, leading to improved function and quality of life. As we delve into strategies for hand recovery, it's essential to remember that the journey is as unique as the individual, and progress may vary from one person to another.
Basics of Hand Rehabilitation
Rehabilitation following a stroke is an intricate blend of science, art, and individual willpower. When it comes to hand rehabilitation, the journey is focused on regaining both function and sensation, ensuring the hand can once again serve its myriad roles, from functional tasks to expressive gestures. To grasp the fundamentals of hand rehabilitation post-stroke, there are a few key concepts and approaches to understand:
Early Intervention is Crucial: The initial period following a stroke is a critical window for rehabilitation. This phase, often termed the 'golden period,' is when the brain is most responsive to therapy and can make the most significant gains. Initiating hand rehabilitation exercises and treatments as soon as medically feasible can result in better outcomes.
Neuroplasticity – The Brain's Remarkable Ability: One of the foundational principles behind rehabilitation is the concept of neuroplasticity. Simply put, it's the brain's ability to reorganize itself by forming new neural connections. While some brain cells may be damaged irreparably due to a stroke, other parts can adapt and take over lost functions. Targeted therapies and exercises can stimulate this reorganization, leading to regained hand functions.
Holistic Approach: Hand rehabilitation is not just about muscle strength or movement. It's equally important to focus on sensory aspects, coordination, and even psychological facets. Ensuring that therapy addresses all these areas will create a more comprehensive recovery.
Customized Therapy: Every stroke patient's experience and needs are unique. While there are general therapies and exercises beneficial for most, it's vital to tailor the rehabilitation process to the individual's specific deficits, goals, and progression rate.
Consistency and Repetition: Recovery is a gradual process. Consistent practice and repetition of exercises are key to retraining the brain and muscles. Over time, these repeated movements can help reinforce the neural pathways associated with hand function.
Integrating Real-Life Activities: Rehabilitation should not be limited to structured therapy sessions. Incorporating real-life tasks and activities that the patient finds meaningful can motivate them and reinforce the functional use of the hand in daily life.
Feedback is Vital: Whether it's through observing one's progress, receiving feedback from a therapist, or using biofeedback tools, understanding how one's hand is responding to therapy can guide the recovery journey and boost morale.
Psychological Support: The emotional toll of a stroke and the subsequent journey of recovery cannot be underestimated. Incorporating psychological support, be it through counseling, support groups, or other means, is essential to address the mental and emotional challenges that come with physical rehabilitation.
In essence, hand rehabilitation after a stroke is a multi-faceted journey. By understanding these basics, patients, caregivers, and therapists can collaborate more effectively, paving the way for the best possible recovery outcomes.
6 Stages of Hand Recovery Post-Stroke (Brunnstrom Stages of Stroke Recovery)
Hand recovery after a stroke is a complex process that typically progresses through several stages. These stages reflect the body's natural healing process and the brain's ability to reorganize itself, known as neuroplasticity. Here's a breakdown of the stages:
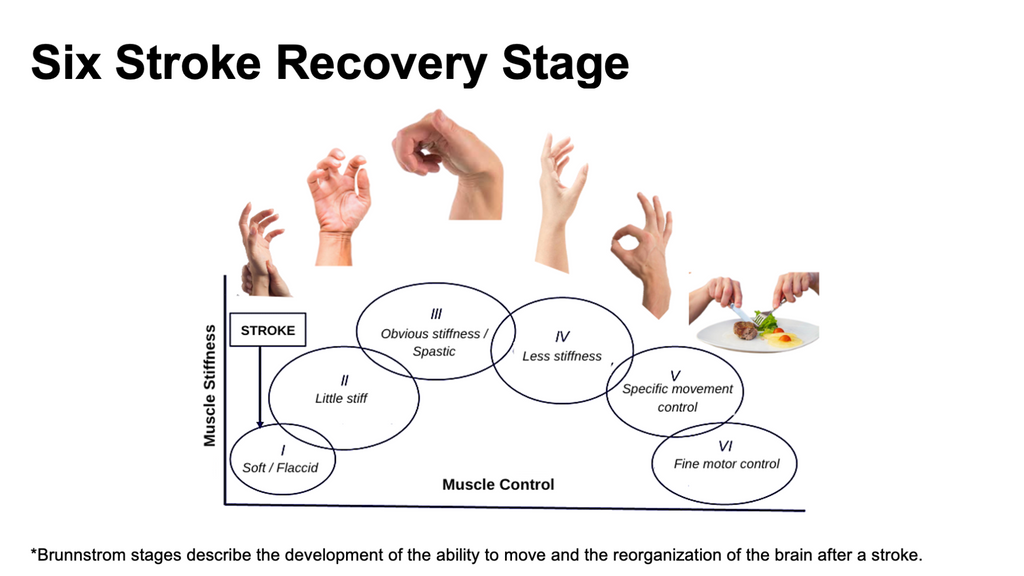
Stage 1. Flaccid Paralysis (or Flaccidity)
This is the initial stage post-stroke. The affected hand muscles become limp or flaccid, leading to an inability to move the hand or fingers. This stage can last from days to several weeks.The sudden interruption of blood flow during the stroke damages certain areas of the brain, resulting in a loss of voluntary muscle control.
Stage 2. Spasticity and the Beginning of Voluntary Movement
Muscles may begin to stiffen or become spastic, leading to involuntary muscle contractions. Some initial and very limited voluntary movements might be noticed, though they may be jerky or uncoordinated. This can persist for weeks to months. The duration varies widely among individuals. As the brain starts healing and forming new connections, it begins to send signals to the affected muscles. However, due to damaged pathways, these signals can sometimes lead to excessive or uncontrolled muscle contractions.
Stage 3. Increased Spasticity and Voluntary Control
While spasticity might increase, making muscles stiffer, there is also a parallel increase in the ability to control voluntary movements. The movement is still not perfect and may be limited. This stage can overlap with the previous and might last for several months. The brain continues its recovery process, with improved but still not perfect signaling to the hand muscles.
Stage 4. Reduced Spasticity and Improved Coordination
Spasticity begins to decrease, leading to a reduction in stiffness and involuntary contractions. There's a notable improvement in hand coordination and function. This stage's timeline varies, but improvements can be seen over months and even years with consistent therapy. Continuous therapy, exercises, and the brain's neuroplasticity play a role in improving motor functions and coordination.
Stage 5. Complex Motor Skill Recovery
At this stage, the individual can perform complex tasks using the affected hand, like buttoning a shirt, writing, or using utensils. Achieving this stage can take months to years and might require persistent and specialized therapies. The culmination of therapy, exercises, and the brain's ability to adapt results in regaining more refined hand functions.
Stage 6. Near-Normal Function (or Plateau)
The affected hand's functions might be close to normal, but there might still be minor deficits compared to the pre-stroke state. While significant improvements might plateau, subtle improvements can continue for years. Continued use of the hand in daily activities, along with specialized exercises, contributes to sustaining and even slightly improving the achieved function.
Rehabilitation Techniques & Strategy Based on the 6 Stages of Recovery in Stroke
Each stage of post-stroke recovery presents its own set of challenges and, subsequently, necessitates specialized rehabilitation interventions. By synchronizing rehabilitation techniques with the evolving needs of the stroke survivor, we not only maximize functional outcomes but also empower individuals to reclaim their independence.
- Stage: Flaccid Paralysis (or Flaccidity)
Techniques:
- Passive Range of Motion (ROM) exercises
- Gentle manual muscle stretching
Strategies:
- Protect the hand from injuries using splints or soft positioning devices.
- Regularly change the hand's position to prevent pressure sores.
- Stage: Spasticity Begins & Limited Voluntary Movement
Techniques:
- Prolonged stretching
- Active-assisted ROM exercises
- Basic neuromuscular techniques
Strategies:
- Begin electrical stimulation to initiate muscle contractions.
- Use of anti-spasticity medications, if prescribed.
- Stage: Increased Spasticity & Voluntary Control
Techniques:
- Active ROM exercises
- Task-specific training for grasping and releasing objects
- Progressive resistance exercises
Strategies:
- Introduce mirror therapy to leverage the brain's mirror neurons for rehabilitation.
- Utilize technology like biofeedback for muscle training.
- Stage: Reduced Spasticity & Improved Coordination
Techniques:
- Advanced neuromuscular retraining
- Hand dexterity and coordination exercises
- Constraint-Induced Movement Therapy (CIMT)
Strategies:
- Integrate activities that focus on quality over quantity, ensuring movements are purposeful and coordinated.
- Utilize functional tasks like buttoning shirts or using utensils.
- Stage: Complex Motor Skills Recovery
Techniques:
- Fine motor skill exercises like bead threading or coin stacking
- Bilateral coordination activities
- Sensory retraining exercises
Strategies:
- Use of virtual reality or augmented reality platforms to simulate real-world hand activities and tasks.
- Incorporate community-based or vocational tasks to integrate the hand back into daily life and work.
- Stage: Near-Normal Function & Refinement
Techniques:
- Precision tasks like handwriting or intricate crafts
- Sensory discrimination activities
- Advanced neuromuscular techniques
Strategies:
- Engage in hobbies or tasks that challenge the hand, like musical instruments or art.
- Continued assessment to identify any lingering deficits and address them through targeted interventions.
It's crucial to emphasize that while these stages provide a general framework, every stroke survivor's journey is unique. Adjustments to techniques and strategies should be made based on individual progress, challenges, and goals. Collaboration among therapists, the patient, and caregivers ensures the best possible outcomes.
Strategies & Techniques Based on Hand Impairment After Stroke
Post-stroke, the landscape of hand function may be dramatically altered, ranging from weakness and spasticity to sensory disturbances or coordination challenges. However, hope emerges when rehabilitation is meticulously aligned with the specific nature of the impairment. This guide delves deep into specialized strategies and techniques designed for various hand impairments following a stroke.

- Hand Weakness:
Techniques:
- Strength Training: Progressive resistance exercises focusing on grip strength and finger flexion/extension.
- Electrical Stimulation : Stimulates weakened muscles, promoting movement and strength.
Strategies:
- Emphasize task-specific training to utilize and enhance muscle strength, such as lifting or carrying objects.
- Hand Spasticity:
Techniques:
- Prolonged Stretching: Helps in reducing muscle tone and maintaining length.
- Splinting: Maintains the hand in a functional position, counteracting spastic posture.
- Botulinum Toxin Injections: Reduces spasticity in specific muscle groups.
Strategies:
- Incorporate neuromuscular techniques that promote voluntary control and inhibit unwanted reflexes.
- Sensory Disturbances:
Techniques:
- Sensory Re-education: Activities like texture recognition, temperature differentiation, and two-point discrimination.
- Desensitization: For hypersensitive areas, using different textures and sensations.
Strategies:
- Engage in tasks that require sensory feedback, such as identifying objects with closed eyes or navigating textured pathways.
- Coordination and Fine Motor Skills Deficits:
Techniques:
- Dexterity Exercises: Tasks like bead threading, coin stacking, and pinching exercises.
- Mirror Therapy: Uses visual feedback to enhance motor control and coordination.
Strategies:
- Integrate activities that challenge coordination, from basic (e.g., turning pages of a book) to advanced (e.g., buttoning or handwriting).
- Hand Edema or Swelling:
Techniques:
- Elevation: Regularly elevating the hand above heart level.
- Compression Gloves: Can help in reducing swelling.
- Manual Lymphatic Drainage: Gentle massage to facilitate fluid movement.
Strategies:
- Maintain active movement within comfort limits to promote fluid circulation.
- Reduced Range of Motion (ROM):
Techniques:
- Passive and Active-Assisted Stretching: Ensures joint flexibility and counteracts contractures.
- Joint Mobilizations: Manual techniques by trained therapists to improve joint movement.
Strategies:
- Incorporate regular movement and stretching intervals throughout the day to prevent stiffness.
For effective hand rehabilitation post-stroke, a combination of these strategies and techniques is typically needed. The approach should be individualized based on assessment findings, patient goals, and feedback during therapy sessions. Collaboration among therapists, patients, and caregivers is essential for maximizing recovery.
Hand Recovery Plan and Timeline After Stroke
The journey of hand recovery post-stroke is neither linear nor predictable for everyone. However, a structured approach, informed by stages of recovery, can illuminate the path forward. This guide seeks to delineate a general roadmap for hand recovery after a stroke, understanding the benchmarks and strategies at each phase.

- Acute Phase (Days 1-7):
Focus: Protection, assessment, and passive movement.
Interventions:
- Gentle passive range of motion exercises to maintain joint flexibility.
- Splinting or positioning to prevent hand deformities.
- Initial assessment of hand functions: grip strength, sensation, reflexes.
Goal: Protect the hand from injury, maintain joint health, and establish a baseline for rehabilitation.
- Subacute Phase (Week 1-4):
Focus: Initiation of active movement and sensory stimulation.
Interventions:
- Assisted and active hand exercises: finger flexion and extension, thumb opposition.
- Sensory re-education techniques, such as textured touch and temperature differentiation.
- Use of assistive devices or adaptive techniques for daily tasks.
Goal: Encourage the return of voluntary movement, improve sensory perception, and foster basic hand functions.
- Early Recovery Phase (Month 1-6):
Focus: Intensive hand rehabilitation and functional task training.
Interventions:
- Progressive strength training exercises for grip and pinch.
- Fine motor skills training: bead threading, coin stacking, and buttoning exercises.
- Mirror therapy or electrical stimulation if indicated.
- Task-specific training, like holding utensils, writing, and self-care tasks.
Goal: Regain functional hand skills, strengthen weakened muscles, and improve dexterity.
- Late Recovery Phase (Month 6-12)
Focus: Refinement of hand skills and community integration.
Interventions:
- Advanced hand therapy exercises targeting specific needs.
- Vocational or hobby-specific training, such as typing, playing musical instruments, or crafting.
- Community-based programs to promote real-world hand function use.
Goal: Achieve a level of hand function that allows return to work, hobbies, and daily activities.
- Chronic Phase (1 year and beyond):
Focus: Maintenance of hand function, adaptive strategies, and quality of life enhancement.
Interventions:
- Periodic therapy sessions to address any lingering issues or refine certain skills.
- Continued practice of daily activities and exercises at home.
- Exploration of advanced assistive technologies or devices if needed.
Goal: Maintain and further enhance hand function, adapt to any residual deficits, and ensure a fulfilling quality of life.
It's crucial to periodically assess the progress and adjust the recovery plan based on the patient's evolving needs. Collaboration among therapists, patients, and caregivers throughout this journey is fundamental for achieving the best possible outcomes for hand function post-stroke.
It is also importance of adopting new technological approaches for enhanced recovery. The rehabilitation landscape is evolving rapidly, with technology playing a significant role in reshaping therapeutic interventions. Harnessing the hand robotic technology is the latest way on how you can use to speed up the recovery process.
Introducing the Techcare Hand Robot (HR-30): The Hand Robotic Rehabilitation Technology.

✅ Enhanced Productivity: Experience a 20X amplification compared to conventional manual rehab methodologies with 1000+ repetition in 60mins
✅ Cover 6 Stage of Rehabilitation Training: A diversified 6-in-1 training module accommodates all stages of recovery, ensuring a tailored approach.
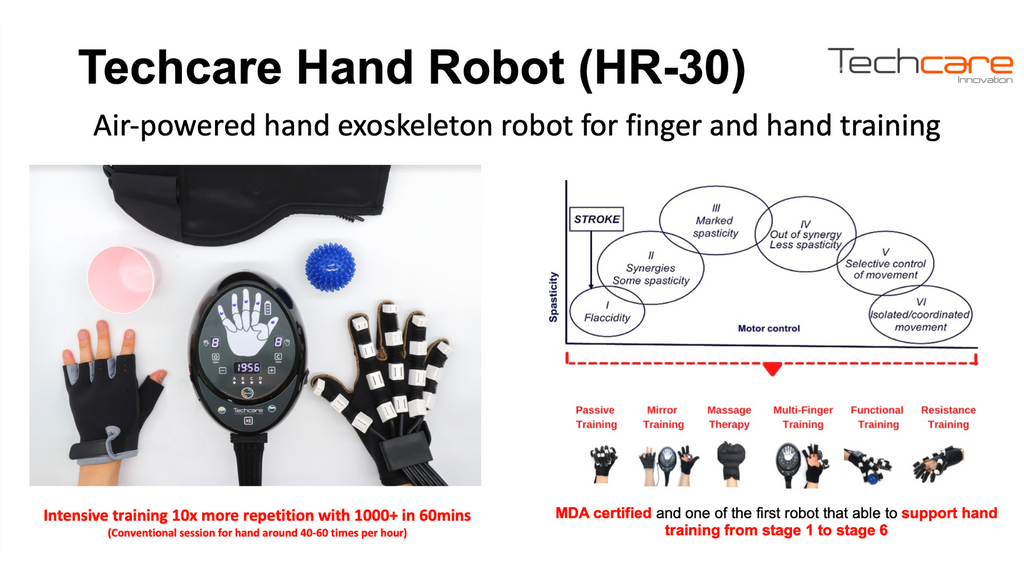
✅ Streamlined Operation: With an intuitive design, setup is achievable in under 3 minutes. Equip the glove, activate the robot, and commence the session.
✅ Specialized Training Professional trained by robotic specialist, ensuring optimal utilization and training outcome.
✅ Local Manufacturer: Two decades deep in rehab robot research and innovation, recognized by 30 distinct innovation awards with local manufacturer support and services
✅ MDA Certified: Meet rigorous standards of safety and efficacy with our Medical Device Authority certification.
Imagine having a dedicated rehab assistant at your beck and call, right in the comfort of your side! Save time, exert less effort, and witness rapid results. A majority of our customers report noticeable improvements after just 1-6 months of continuous treatment sessions.
The Techcare Hand Robot (HR-30) had been used by reputable professional in the nation including hospital and rehabilitaiton center. It doesn't merely act as a tool; it's an extension of hand rehabilitation,if use correctly with guided professional it will revolutionize your recovery journey.
It provide both home and clinical package. Reach out us directly to access exclusive offers now!
Whatsapp : Techcare Customer Specialist
Disclaimer :
The content provided in this blog, including all text, images, and other materials, is for informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read on this blog.

